Table of Contents
- Understanding the Basics: What is SILK Eye Surgery?
- The LASIK Approach: A Deep Dive into Its Mechanism
- Comparative Analysis: Corneal Strength Post-Surgery
- Key Comparison Table: SILK vs LASIK
- The Science Behind SILK’s Superior Corneal Preservation
- What Is the Recovery Timeline After SILK?
- Choosing the Right Procedure: SILK vs LASIK
- Conclusion
- FAQs
In the world of advanced vision correction, LASIK has transformed millions of lives by reducing dependence on glasses and contact lenses. However, even as LASIK continues to evolve, new ophthalmic technologies are setting higher standards for precision and safety. One such revolutionary advancement is the Smooth Incision Lenticule Extraction (SILK) procedure. As patient expectations for visual outcomes and long-term eye health continue to rise, it is imperative to understand how SILK outperforms traditional LASIK, particularly in preserving corneal strength, reducing complications, and enabling patients to resume their lives with renewed clarity.
Understanding the Basics: What is SILK Eye Surgery?
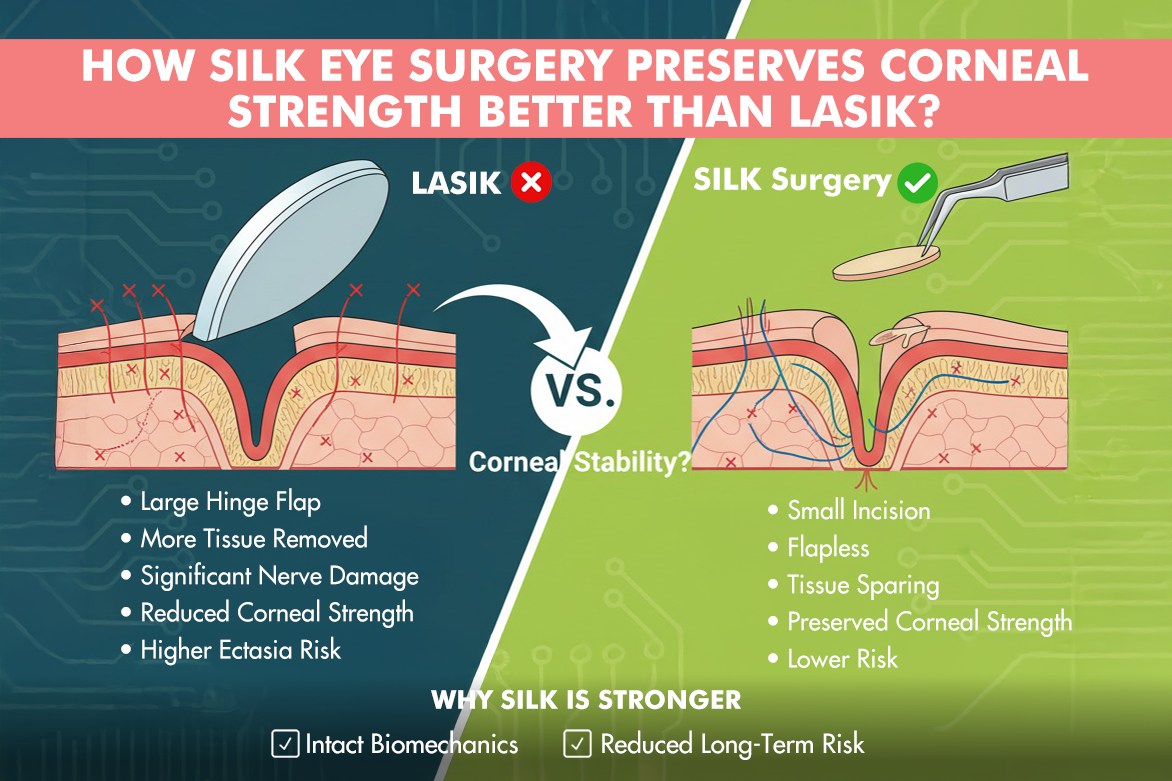
SILK eye surgery represents the next frontier in minimally invasive refractive surgery, especially for treating myopia and astigmatism. During SILK, a femtosecond laser creates a precisely shaped lenticule, a tiny, lens-shaped piece of tissue, within the corneal stroma. This lenticule is extracted through a microscopic incision (typically 2–4 mm), which is much smaller than the flap created in conventional LASIK. By eliminating the formation of a wide corneal flap, SILK leaves the anterior corneal layers largely untouched, thereby maintaining greater corneal integrity.
Clinical facts about SILK
- Minimally invasive, “flapless” technology preserves up to 30% more biomechanical strength compared to flap-based laser procedures.
- The small incision reduces disturbance to corneal nerves, translating to lower rates of post-surgical dry eye and faster nerve regeneration.
- Suitable for a wider range of patients, including those with thinner corneas or lifestyle requirements that heighten the risk of trauma.
The LASIK Approach: A Deep Dive into Its Mechanism
LASIK (Laser-Assisted In Situ Keratomileusis) has been a cornerstone of refractive surgery for decades, helping countless patients achieve spectacle independence. The essence of LASIK lies in the creation of a thin, hinged corneal flap, typically 20 mm or more, using a microkeratome blade or a femtosecond laser. The surgeon lifts this flap, reshapes the underlying corneal tissue with an excimer laser, and repositions the flap over the treatment zone. The interface heals over time, forming a natural bandage.
Clinical facts about LASIK:
- Rapid visual recovery: Most patients notice improved vision within hours to a day.
- Versatile: Suitable for correcting myopia, hyperopia, and astigmatism.
- Customizable treatments: Advancements like wavefront-guided or topography-guided LASIK have further improved outcomes for patients with irregular corneas.
Potential downsides of LASIK surgery:
- The corneal flap permanently alters corneal structure, which may reduce biomechanical strength by 30-40%.
- Flap-related complications, although rare, can include dislocation, folds, or epithelial ingrowth.
- Slightly increased risk of postoperative dry eye and altered corneal sensation.
Comparative Analysis: Corneal Strength Post-Surgery
A fundamental concern in all refractive surgery is ensuring the long-term biomechanical integrity of the cornea. The cornea’s strength is crucial for withstanding intraocular pressure and maintaining its natural curvature and shape, which are essential for crisp, stable vision. LASIK, despite its reliability, inherently weakens the cornea by creating a flap that severs anterior corneal lamellae, the strongest layers of the cornea. This can, in some cases, result in complications such as corneal ectasia, where the corneal wall progressively becomes thinner and begins to bulge, severely impacting vision.
- By contrast, SILK eye surgery works through a much smaller incision, which leaves the majority of the corneal layers, particularly the tough anterior stroma, unaltered. As a result:
- SILK procedures show a 50–70% lower risk of postoperative corneal ectasia compared to LASIK.
- The preservation of the anterior stromal lamellae plays a decisive role in maintaining corneal stability and biomechanical strength.
- Scientific studies using corneal biomechanics analyzers (such as Corvis ST or Ocular Response Analyzer) consistently reveal higher post-operative corneal resistance factors for SILK compared to LASIK.
Key Comparison Table: SILK vs LASIK
| Feature | LASIK | SILK |
| Incision/Dissection | Flap 20mm+ | Micro-incision 2–4mm |
| Anterior Stromal Preservation | Reduced | Maximally Preserved |
| Dry Eye Risk | Moderate | Lower |
| Risk of Corneal Ectasia | Elevated in risk groups | Significantly reduced |
| Suitable for Thin Corneas | Limited | Expanded eligibility |
| Flap-related Complications | Possible | None |
The Science Behind SILK’s Superior Corneal Preservation
To understand why SILK is best at corneal preservation, one must know the cornea’s anatomy. The strongest biomechanical tissue lies in the anterior stromal layers; by not bombarding the laser fire on these, SILK surgery maintains the cornea’s resilience against intraocular pressure and environmental stresses for years after surgery. In contrast, LASIK’s wide flap cuts through critical lamellae, resulting in a lingering loss of strength. Further, SILK’s micro-incision means fewer nerves are transected, contributing to quicker corneal nerve regeneration, supporting tear film stability, and reducing postoperative dryness. It also enhances long-term comfort and reduces the need for lubricating drops.
Recent clinical research also shows that SILK’s method of tissue removal, without vaporizing tissue, as in excimer laser-based surgeries, minimizes thermal and structural changes in the surrounding corneal cells. Additionally, advanced SILK platforms utilize real-time eye tracking and sophisticated femtosecond lasers, ensuring pinpoint accuracy at every step.
SILK Surgery corneal preservation mechanism:
- Distribution of biomechanical stress within the cornea post-SILK remains more natural and uniform, crucial for maintaining physiological curvature.
- SILK’s approach supports greater predictability and stability of refractive outcomes, key for patients with high prescriptions or thinner corneas.
What Is the Recovery Timeline After SILK?
SILK surgery is renowned for its rapid, gentle recovery profile. Most patients experience marked improvements in vision within a single day, and the absence of a wide corneal flap means the eye’s natural barrier function is restored much sooner.
Recovery features
- Most patients return to work and daily routines within 24–48 hours.
- There is less post-surgical pain, irritation, or foreign body sensation compared to flap-based methods.
- Activities with a higher risk of eye trauma (sports, swimming) are often resumed more quickly since there is no flap dislocation risk.
Key postoperative care practices include
- Strict adherence to prescribed antibiotic and steroid drops.
- Avoid eye rubbing and heavy lifting in the early days.
- Attend scheduled follow-up visits for optimal results.
Patient-reported outcomes, as well as large clinical trials, reveal a high degree of satisfaction with both the recovery process and long-term visual results after SILK.
Choosing the Right Procedure: SILK vs LASIK
The decision between SILK vs LASIK is multifactorial and best made after a comprehensive diagnostic evaluation by a refractive surgeon. Factors to consider include:
- Corneal thickness and topography: SILK is advantageous for those with thinner, irregular, or high-risk corneas.
- Lifestyle: For athletes, military personnel, and individuals with physically demanding jobs or hobbies, SILK’s flapless technique minimizes trauma-related risks.
- Degree and type of refractive error: While LASIK is effective for a broader range of refractive errors, technological advances now allow SILK to safely treat moderate to high myopia and certain types of astigmatism.
- Patient preferences: Some value the rapid recovery and proven track record of LASIK, while others prioritize structural preservation and reduced complication risk found in SILK.
At Planet Lasik by Centre For Sight, patients benefit from advanced preoperative diagnostics, including Pentacam mapping, corneal biomechanics assessments, and individualized counseling to clarify the risks and advantages based on personal needs.
Conclusion
Advancements in eye surgery with procedures like SILK are reshaping the landscape of vision correction, providing lasting clarity while prioritizing the safety and biomechanical health of the eye. By understanding the clear clinical differences and considering one’s unique ocular profile, individuals are better positioned to make informed choices for lifelong visual freedom. As technology continues to evolve, patients can rest assured that their future vision is in the hands of experienced professionals and pioneering techniques dedicated to both immediate results and long-term corneal wellness.
FAQs
Is SILK suitable for people with thin corneas?
SILK is considered safer for certain patients, particularly those with thinner corneas, due to its minimally invasive nature and better preservation of corneal strength.
How does visual clarity compare between SILK and LASIK?
Visual clarity achieved with SILK is comparable to LASIK, with many patients reporting excellent outcomes.
How soon can I return to normal activities after SILK?
Recovery after SILK is typically swift, with most individuals returning to normal activities within a few days.
Does SILK reduce the risk of corneal ectasia?
Importantly, SILK significantly reduces the risk of corneal ectasia compared to LASIK, making it a preferred option for those concerned about corneal health.