Table of Contents
- Understanding the Basics: What is Keratoconus?
- Risks of Performing LASIK on Keratoconus Suspects
- The Pillars of Proper LASIK Screening at Planet Lasik
- Safer Alternatives to LASIK for High-Risk Patients
- Conclusion
- FAQs
In the world of vision correction, LASIK has long been a revolutionary surgery, offering freedom from glasses and contact lenses. It has provided crystal-clear vision to millions of people, transforming their daily lives. However, like any advanced medical procedure, its success significantly depends on one crucial factor: patient selection. Not every person is a suitable candidate for LASIK, and for those with a condition known as Keratoconus, or even a suspicion of it, the stakes are incredibly high.
This blog is a deep dive into why a comprehensive screening for keratoconus before LASIK is not just a formality but the single most important step for anyone considering this life-changing procedure, especially for those who are Keratoconus suspects.
Understanding the Basics: What is Keratoconus?
Keratoconus is a progressive, non-inflammatory eye disorder that affects the cornea, the clear, dome-shaped front surface of your eye. In a healthy eye, the cornea is strong and maintains its shape. In a person with Keratoconus, the cornea begins to thin and weaken, leading to a bulge outward into a cone-like shape. This change in shape distorts the way light enters the eye, leading to significant vision problems. Its symptoms can include:
- Blurred or distorted vision
- Increased sensitivity to light and glare
- Frequent changes in eyeglass prescriptions
- Difficulty with night driving due to halos and starbursts
The condition typically begins to appear during puberty or early adulthood and can progress for 10 to 20 years before stabilizing. Early detection is key to effective management and preventing further vision loss.
Who Is a Keratoconus Suspect?
While some people have clear, clinical signs of Keratoconus, others have a subclinical form, often referred to as a “keratoconus suspect”. These individuals do not yet show the major signs and symptoms that are obvious during a routine eye exam, but have subtle, tell-tale indicators that can only be picked up by advanced diagnostic equipment. A person may be classified as a Keratoconus suspect if their corneal topography or tomography scans show subtle irregularities such as:
- Asymmetric bow-tie pattern: A slight imbalance in the curvature of the cornea, which is a classic sign of early Keratoconus.
- Subtle corneal thinning: The cornea is not yet dangerously thin but shows a measurable reduction in thickness in specific areas.
- Posterior corneal elevation: An upward bulge on the back surface of the cornea, which is one of the earliest signs of the disease and is only detectable with advanced tomography.
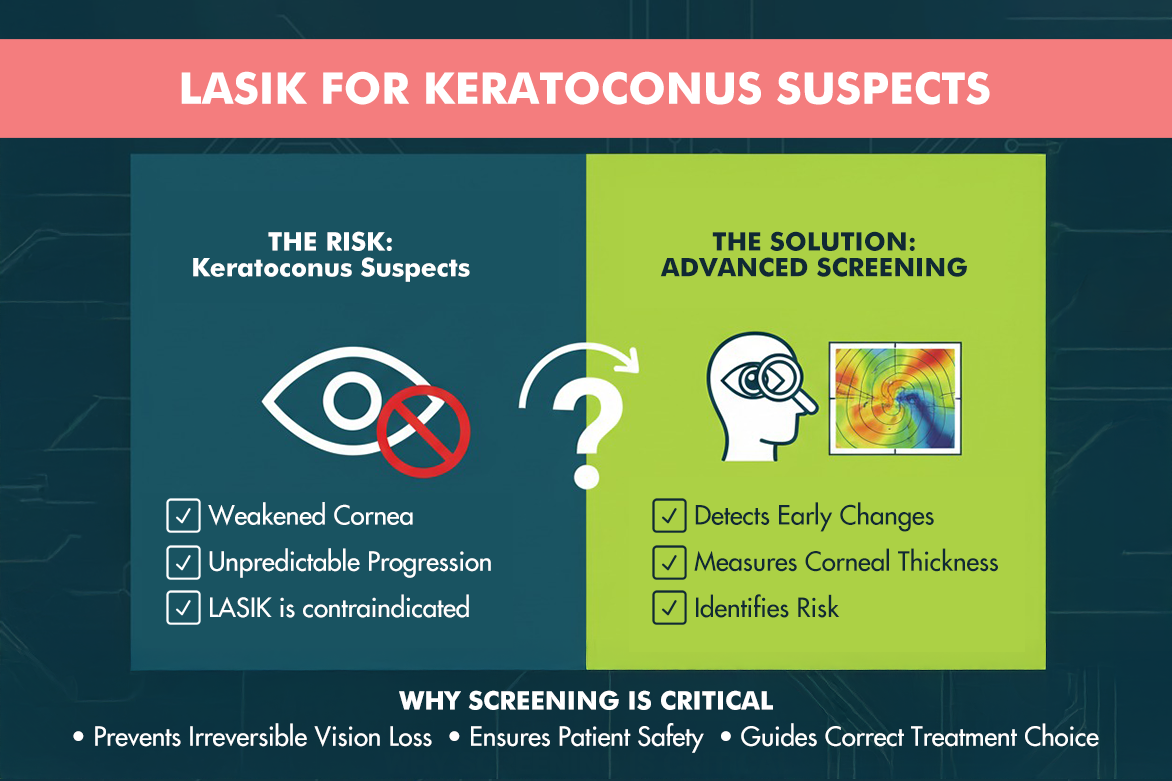
Risks of Performing LASIK on Keratoconus Suspects
The core of the LASIK procedure involves using an excimer laser to remove a microscopic amount of corneal tissue to reshape the cornea and correct refractive errors. While this is a safe and effective procedure for a structurally healthy cornea, it can be disastrous for a cornea that is already compromised.
The single most significant LASIK risk keratoconus suspect patients face is the potential for developing post-LASIK ectasia. This condition is a worsened, and often more rapid, progression of Keratoconus triggered by the surgical procedure itself. Here’s why this happens:
Compromised Corneal Integrity: The excimer laser removes tissue from the cornea’s central layer (stroma) to correct vision. In a person who is a Keratoconus suspect, this already weakened cornea cannot withstand the structural changes, leading to a breakdown of its biomechanical integrity.
Progressive Bulging: With the cornea’s strength compromised, the internal pressure of the eye causes the thinned cornea to bulge forward in an uncontrolled manner. This leads to a severe, unpredictable change in the cornea’s shape, resulting in significant and often irreversible vision loss.
The severity of post LASIK ectasia risk is directly tied to the thoroughness of the pre-operative screening. In the past, when diagnostic tools were less advanced, ectasia was a more common complication.
The Pillars of Proper LASIK Screening at Planet Lasik
At Planet Lasik by Centre For Sight, our commitment to patient safety and long-term vision health is unwavering. This is why our screening process goes far beyond a basic eye chart test. We utilize the state-of-the-art diagnostic tools to ensure every candidate is thoroughly evaluated.
- Corneal Topography
Corneal topography is a non-invasive imaging technique that creates a 3D map of the cornea’s front surface. It’s like a geographical map, but for your eye, revealing any irregularities or steepening that could indicate early signs of Keratoconus. - Corneal Tomography (The Gold Standard)
While topography is essential, it only maps the front surface. For a truly comprehensive understanding of corneal health, we rely on Corneal Tomography, performed by advanced machines like the Pentacam. A Pentacam uses a rotating Scheimpflug camera to create a detailed 3D reconstruction of the entire cornea, including both the front and back surfaces, as well as its thickness from edge to edge.
- Corneal Pachymetry
Corneal Pachymetry is the measurement of the cornea’s thickness. While this is a component of tomography, it is a critical measurement on its own. If the cornea is too thin, it may not have enough tissue to safely undergo LASIK without the risk of weakening the structure. - Wavefront Analysis (Aberrometry)
It helps identify higher-order aberrations, which are vision distortions not correctable with standard glasses or contact lenses. In some cases, an increase in these aberrations can be a red flag for a changing corneal shape, hinting at early Keratoconus.
Safer Alternatives to LASIK for High-Risk Patients
Discovering you are a Keratoconus suspect is not a dead end for your vision correction journey. If our screening reveals even the slightest hint of this condition, we will immediately rule out LASIK and discuss safer alternatives.
- Corneal Collagen Cross-Linking (CXL)
CXL is a minimally invasive procedure that is the gold-standard treatment for halting the progression of Keratoconus. Using a combination of a vitamin B2 solution (riboflavin) and ultraviolet (UV) light, it creates new links between the collagen fibers in the cornea, making it stronger and more rigid. CXL is a highly effective treatment for stabilizing the cornea and preventing further vision loss.
- Implantable Collamer Lens (ICL)
For high-risk patients who are not suitable for LASIK, an ICL is an excellent option. An ICL is a thin, flexible lens that is surgically implanted inside the eye, behind the iris and in front of the natural lens. This procedure corrects vision without removing any corneal tissue, making it a safe and effective solution for patients with thin corneas or Keratoconus.
- Advanced Surface Ablation (PRK)
For certain patients with very mild, stable Keratoconus and an otherwise healthy cornea, PRK (Photorefractive Keratectomy) may be considered. PRK involves reshaping the cornea’s surface without creating a flap. It is often combined with CXL to provide both vision correction and corneal strengthening.
Conclusion
The journey to clear vision is an exciting one, but it must be taken with caution and expert guidance. At Planet Lasik by Centre For Sight, our philosophy is simple: we will never perform a procedure that we believe is not in your best long-term interest. By investing in the most advanced diagnostic technology and prioritizing a comprehensive LASIK keratoconus screening, we ensure that our patients not only achieve clear vision today but maintain healthy eyes for a lifetime.
FAQs:
What are the main signs that I might be a Keratoconus suspect?
You may have a family history of the condition, you frequently rub your eyes, or you have noticed your glasses prescription changing very rapidly. Only a comprehensive screening can confirm a diagnosis.
Is post LASIK ectasia common?
With modern screening technology, the incidence of post-LASIK ectasia is very low. However, it is a serious complication, and the only way to avoid it is through a meticulous pre-operative screening process.
Is SMILE surgery an option for Keratoconus suspects?
While SMILE is considered safer than traditional LASIK for some patients with thin corneas, it is not a recommended procedure for those who are definitively diagnosed with Keratoconus or are considered high-risk suspects.
Can Keratoconus be cured?
Treatments like Corneal Collagen Cross-Linking (CXL) are highly effective at halting the progression of the disease, preventing further vision loss, and stabilising the cornea.
Why is my doctor recommending a Pentacam scan specifically?
The Pentacam provides the most detailed information about your cornea’s front and back surfaces and its thickness. It helps to identify the subtle signs that a simple topography scan might miss.